Labor and Employment Alert: Summaries of Benefits and Coverage (SBCs) Back on the Schedule and Other Employee Benefits News
A short history of SBCs
An SBC is a standardized explanation of health coverage intended to help 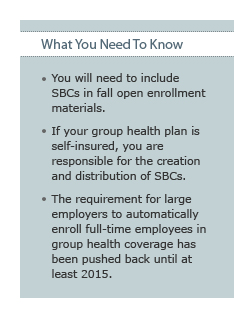 individuals make apples-to-apples comparisons of their options for health coverage. The Internal Revenue Service, Department of Labor and the Department of Health and Human Services (the Departments) published proposed SBC rules and an SBC template on August 22, 2011. Those rules would have required employers to provide SBCs to employees enrolling in health coverage on and after March 23, 2012. But then the Departments announced, on November 17, 2011, that they would push back the SBC effective date while they considered the problems pointed out by the public.
individuals make apples-to-apples comparisons of their options for health coverage. The Internal Revenue Service, Department of Labor and the Department of Health and Human Services (the Departments) published proposed SBC rules and an SBC template on August 22, 2011. Those rules would have required employers to provide SBCs to employees enrolling in health coverage on and after March 23, 2012. But then the Departments announced, on November 17, 2011, that they would push back the SBC effective date while they considered the problems pointed out by the public.
The revised rules and template were published on February 9, 2012 (available at http://www.dol.gov/ebsa/healthreform/). The revised rules and template are an improvement over the originals, but are still going to pose challenges to employers.
When does your SBC need to be ready?
The new effective date for the SBC rules is based on the first open enrollment period and plan year starting on or after September 23, 2012 (six months later than the original March 23, 2012 effective date). The SBC rules apply to:
- The first open enrollment period starting on or after September 23, 2012; and
- The first plan year starting on or after September 23, 2012, for employees enrolling at some time other than open enrollment (for example, new hires enrolling after an initial waiting period or employees enrolling in connection with marriage, birth, adoption, loss of other coverage or other event).
If your enrollment year and plan year are the calendar year, the SBC rules will apply to your next open enrollment window (generally conducted in the fourth quarter of 2012) and to all enrollments on or after January 1, 2013.
SBCs are required for both grandfathered and non-grandfathered health plans. There is no exception for small employers.
When do SBCs have to be distributed?
After the effective date:
- SBCs have to be included in open enrollment materials. It is not clear whether the distribution will need to be at least 30 days before the first day of the enrollment period. We will watch for the Departments to clarify this point.
- If you do not hold an annual open enrollment, you have to distribute SBCs at least 30 days before the first day of each plan year.
- SBCs have to be included in enrollment materials provided to newly eligible employees.
- Special rule for special enrollment: An eligible employee has the right to enroll himself or herself (and family members) in a group health plan in connection with special enrollment events such as marriage, birth, adoption, placement for adoption, loss of other coverage and gaining or losing eligibility for certain Medicaid and CHIP programs. You have to provide an SBC within 90 days after a special enrollment. This is also the deadline for providing a summary plan description to new enrollees.
- If a participant requests an SBC, you must provide it as soon as practicable but no later than seven business days of the request. (The original rule would have required you to provide the SBC within seven calendar days of a request.)
- If you make a material change to your group health plan that impacts the information in an SBC and that change takes effect other than at the beginning of an enrollment year, you must provide 60 days advance notice of the changes to the SBC.
Who is responsible for creating and distributing SBCs?
Responsibility for creating and distributing SBCs depends on whether your group health plan is insured or self-insured.
- If your group health plan is insured, the insurer will create the SBC. You can allocate responsibility for distributing the SBC to either the insurer or your plan, but both the insurer and the employer can be penalized for the failure to provide the SBC when required.
- If your group health plan is self-insured, you are responsible for creating and distributing SBCs. Your claims administrator may assist but the employer, as plan sponsor, remains legally responsible. Please let us know if you want us to help create your SBCs or review them for accuracy.
Content
The Department once again provided a template, text for insertion and instructions. Generally, the creation of an SBC is a fill-in-the-blanks exercise where you transfer your group health plan design onto the template. You must follow the prescribed layout, font size (12 point), and (with one exception) wording. What’s new is that if the wording does not accurately describe one or more plan terms, you must use your best efforts to come up with something else that would accurately describe the terms.
The new template is an improvement over the original version. The insurance terminology has been changed so that the template is more appropriate for a self-insured plan. We no longer need to include the premium (cost) so that fewer SBC amendments may be needed.
An SBC may be provided either as a stand-alone document or in combination with other summary materials (like a summary plan description) if the SBC information is intact and prominently displayed at the beginning of the materials, such as immediately after the table of contents in an SPD.
If you offer more than one option for health coverage, you will need a separate SBC for each option. Only the SBC for employees’ current options have to be provided during open enrollment but, as a practical matter, we anticipate employers may choose to provide SBCs for all available options.
You do not need SBCs for so-called “excepted benefits” (such as dental or vision coverage when it is either separately insured or, if self-insured, separately elected and subject to a separate employee contribution).
Expect changes to the template for 2014.
Other Employee Benefits News
Automatic enrollment pushed back
Large employers (in this context, employers with 200 or more full-time employees) will have to automatically enroll full-time employees in group health coverage. Because of the numerous issues that will have to be worked out to make this requirement operational, the Department of Labor previously told us to expect the requirement to go into effect in 2014 but not before. Now, the Department of Labor has pushed automatic enrollment back at least another year. Automatic enrollment will not be required before 2015.
Full-time status and waiting periods in 2014
Starting in 2014, large employers (in this context, employers with 50 or more full-time employees) will be penalized for failing to offer group health coverage to all full-time employees. A full-time employee is one who works, on average, 30 hours per week. The determination of full-time status will be made on a retrospective basis, by counting hours during a look-back period of no more than 12 months.
Another requirement going into effect in 2014 is a 90-day maximum on waiting periods to enroll in group health coverage.
New FAQs in DOL Technical Release 2012-01 describe the Departments’ current thinking on the interplay between the determination of full-time status and the 90-day cap on waiting periods. Most importantly, an employer will not be subject to penalties for failure to offer group health coverage to an employee during his or her first three months of employment. In addition, if an employer limits eligibility for its group health plan to full-time employees, the 90-day waiting period will start when an employee enters the eligible class (i.e., full-time employees). This would mean:
- If an employee does not work full-time during the first three months of employment, the employer will not be subject to penalties for failing to offer health coverage during the employee’s first six months of employment (and potentially beyond).
- If an employee works full-time during the first three months of employment and that schedule is reasonably representative of the average hours the employee is expected to work on an annual basis, the employer must treat the employee as full-time at the end of the three-month period and will be subject to penalties if group health coverage is not offered at the end of the three-month period.
- If an employee works full-time during the first three months of employment but that schedule is not reasonably representative of the average hours the employee is expected to work on an annual basis, the employer can take an additional three-month period to determine whether the employee is or is not full-time. In such a case, the employer will not be subject to penalties for failing to offer health coverage during the employee’s first six months of employment (and potentially beyond). This rule may be especially helpful to companies that might hire employees to work more hours during a busy season (or during initial training) and then fewer hours throughout the balance of the year.
Please let us know if you want more details about the Departments’ emerging vision of group health coverage in 2014.
_______________________
IRS CIRCULAR 230 DISCLOSURE: In order to ensure compliance with requirements imposed by the U.S. Internal Revenue Service, we inform you that any federal tax information contained in this communication (including any attachments) is not intended or written to be used, and it cannot be used, by any taxpayer for the purpose of (i) avoiding penalties that may be imposed under the U.S. Internal Revenue Code; or (ii) promoting, marketing, or recommending to another person, any transaction or other matter addressed herein.
This client alert is for general information purposes and should not be regarded as legal advice.



