Labor and Employment Alert: States to Define "Essential Health Benefits" and Other Employee Health Benefits News
What are essential health benefits?
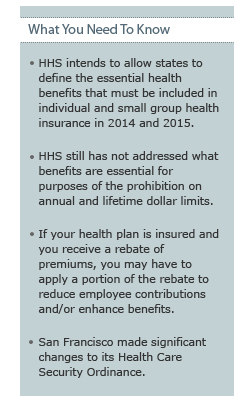 Starting in 2014, every non-grandfathered individual health insurance policy and insured small employer group health plan will have to cover essential health benefits. (In this context, a small group plan is generally a plan sponsored by an employer with no more than 50 employees.) But, what health benefits are – and are not – essential? The Patient Protection and Affordable Care Act (PPACA) provides some parameters. However, PPACA assigns the task of coming up with the actual definition of essential health benefits to the Secretary of the Department of Health and Human Services (HHS). In a Bulletin issued December 16, 2011, HHS proposed to delegate its authority to the states. The delegation would allow HHS to avoid making potentially unpopular decisions about specific benefits.
Starting in 2014, every non-grandfathered individual health insurance policy and insured small employer group health plan will have to cover essential health benefits. (In this context, a small group plan is generally a plan sponsored by an employer with no more than 50 employees.) But, what health benefits are – and are not – essential? The Patient Protection and Affordable Care Act (PPACA) provides some parameters. However, PPACA assigns the task of coming up with the actual definition of essential health benefits to the Secretary of the Department of Health and Human Services (HHS). In a Bulletin issued December 16, 2011, HHS proposed to delegate its authority to the states. The delegation would allow HHS to avoid making potentially unpopular decisions about specific benefits.
Under the HHS proposal, each state would select one of the following as its benchmark plan:
- One of the three largest small group plans in the state;
- One of the three largest state employee health plans;
- One of the three largest federal employee health plan options; or
- The largest HMO plan offered in the state's commercial market.
The benchmark plan (with some adjustments) would serve as the standard for the scope of essential health benefits for non-grandfathered individual health insurance and small employer group health plans in the state for 2014 and 2015. Thus, under the HHS Bulletin, what essential benefits must be covered by a non-grandfathered individual insurance policy or insured small group health plan will vary by state depending on the benchmark plan selected by that state. HHS expects to revisit the issue for 2016.
How does HHS' delegation impact dollar limits on essential health benefits?
Self-insured group health plans are not required to cover all essential health benefits. The same is true for large employer group health insurance policies (although they remain subject to state insurance law). However, PPACA prohibits all health plans from having annual and lifetime dollar limits on essential health benefits. For that reason, the definition of essential health benefits is relevant to the self-insured plans and large employer group health insurance policies.
The HHS Bulletin did not address whether and how the specific benefits, limits, and exclusions in the states' benchmark plans would serve as the standard for determining what benefits may and may not be subject to annual and/or lifetime dollar limits. Pending additional guidance, group health plan sponsors are permitted to continue to apply a good faith reasonable interpretation of what is and is not an essential health benefit taking into account the following categories of benefits:
- Ambulatory patient services;
- Emergency services;
- Hospitalization;
- Maternity and newborn care;
- Mental health and substance use disorder services, including behavioral health treatment;
- Prescription drugs;
- Rehabilitative and habilitative services and devices;
- Laboratory services;
- Preventive and wellness services and chronic disease management; and
- Pediatric services, including oral and vision care.
We expect that not all benefits within the categories will be deemed essential since the essential health benefits package is supposed to be "equal to the scope of benefits provided under a typical employer plan." Please let us know if you want more details.
Remember that the prohibition on annual and lifetime dollar limits does not impact other types of limits. For example, if chiropractic care is deemed to be essential, your plan would not be permitted to impose a $2,000 annual limit on chiropractic care. However, you could impose a 30-visit annual limit – or exclude chiropractic care entirely.
Is your group health plan insured?
The medical loss ratio requirements of PPACA specify that, on average, a specified percentage of health insurance premiums must be spent on medical claims and activities that improve health care quality. The percentage is 80%for individual health insurance and small group plans and 85% for large group plans. In this context, a large group plan is generally a plan sponsored by an employer with more than 50 employees.
An insurance company is required to calculate a separate medical loss ratio for each market (individual, small group, and large group) in each state. The formula for calculating a medical loss ratio is:
[incurred claims + expenditures for health care quality activities]───────────────────────────────────────────────────
[earned premiums ― federal and state taxes and licensing and regulatory fees]
If your insurer fails to meet its medical loss ratio target in your state in 2011, it will rebate a portion of your 2011 premiums by August 1, 2012. The insurer will also send detailed notices to current participants. It is our understanding that rebates are expected to be infrequent.
If your company receives a rebate, please do not assume the company may keep the entire amount. The Department of Labor has published guidance explaining how to determine what portion of a rebate must be applied to reduce employees' future contributions and/or benefit enhancements. For example, if your employees pay 20% of the premium cost for coverage, you will generally need to apply 20% of the rebate to reduce future contributions or provide benefit enhancements. You will not be required to apply the rebate to the same employees whose coverage generated the rebate. If your company receives a rebate and you need assistance determining how and when it may be applied, please let us know.
Do you have employees in San Francisco?
If you have employees in San Francisco, you are no doubt familiar with the San Francisco Health Care Security Ordinance (the HCSO). In November 2011, the City amended the HCSO and those amendments are effective January 2012. Companies that have been complying with the HCSO by contributing to health reimbursement arrangements are subject to a number of new requirements. All companies with employees in San Francisco have to post the new 2012 Official OLSE Notice at worksites. Please let us know if you have questions.



